Let’s divide the world into two influences – internal and external. Let’s add to the two influences one key assumption: both factors change forever at varying rates.
Internal factors originate at the core of us, the individuals. They include our interests and passions, our wants and needs, as well as our “age and stage” qualities such as caring responsibilities, health, and financial motivations. These elements change at rates that are specific to each person and that, although influenced by external factors, are about how we interact with our world. They make up the strengths and dynamic energy of health care human resources.
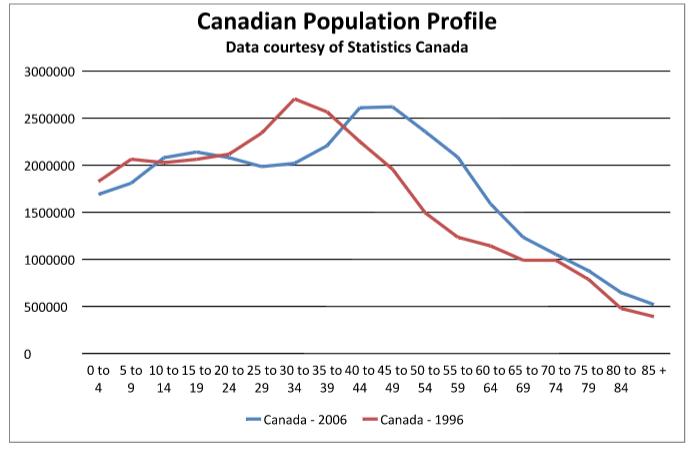
External factors include broad elements of change such as technology, politics, globalization, economics, demography, labour market and social trends. These elements change constantly and interact with each other to compound change. They inform our economy, our funding models, social structures and policy.
We are all obliged to respond to both internal and external influences in a very careful balancing act. We may all fall into habits of regarding one influence over another; as individuals we may become highly tuned into our internal influences at the expense of external, and as organizations we may become habituated to satisfying external demands at the expense of internal.
To make this careful balance function optimally for both the individual and the organization, we are obliged to do three important things simultaneously: understand ourselves very well, keep an eye on change in the world around us, and respond proactively. This juggling of these three distinct functions is difficult and critical to success. We must be fully in tune with our own changing motivations, passions and responsibilities with a clear sense of our own preferred future. At the same time we need to keep our finger on the pulse of trends influencing our work as well as workplace objectives and challenges. It is within the intersection of these internal and external influences that remarkable opportunity waits. Our proactive choices and actions need to be accurately and steadily informed by both sides of the balance so that we can capitalize on opportunity and become leaders in the delivery of quality health care.
The foundation for this balancing act is clear, regular, reciprocal communication. This means that as individuals we need to clearly communicate our passions and interests, changing motivators in our lives, and our desires for next steps at work. As organizations we must articulate trends influencing our work, emerging challenges and goals, as well as clearly voice our vision. It really means that we must listen intently for the harmonies between these two seemingly disparate voices in order to recognize and act upon emerging realities quickly, decisively and with a deep sense of genuine collaboration.